779
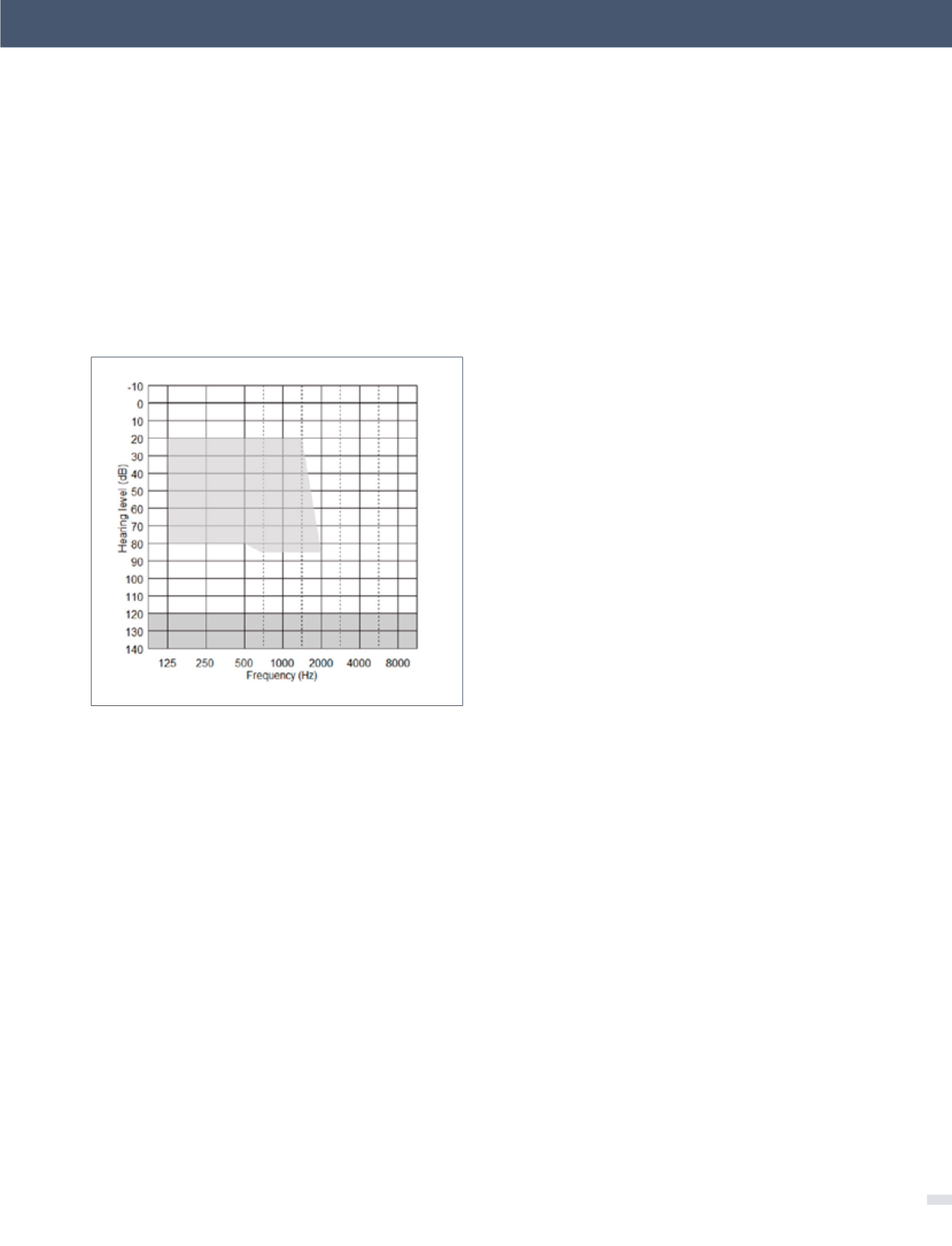
The acoustic component (ACO) of the CP900 processor
may be fitted or removed at any time, but its effective use
depends on the degree of residual postoperative acoustic
hearing, which cannot be reliably predicted before implan-
tation. Indications for use of the ACO are provided by the
fitting range shown in Figure 3 below. Post-operative
thresholds falling within the shaded range indicate frequen-
cies that can be amplified by the CP910/920 in EAS mode.
The influences of device design and surgical
technique on hearing preservation
As preservation of low frequency hearing is a pre-requi-
site of successful use of EAS, this pivotal topic continues to
receive much attention through both basic research and
clinical studies. Findings from these studies have shown
that hearing preservation is dependent on several distinct
factors, particularly: (i) CI electrode design, (ii) surgical tech-
nique, and (iii) patient factors such as degree of residual
hearing.
The concept of “soft surgery” was first introduced by Lehn-
hardt (20), and incorporated a range of guidelines intended
to minimize cochlear trauma, including opening the ST as
late as possible, avoiding suction of perilymph, use of lubri-
cants such as Healon® and slow insertion of the electrode
array. The original aim of soft surgery was to minimize
damage to the cochlea in general and the neural substrate
in particular, in the anticipation of achieving more effective
electrical stimulation. However, most of these principles are
equally valid for hearing (hair cell) preservation. In addition,
surgeons attempting hearing preservation will often try to
avoid drilling into the endeosteum and the use of intra-
venous and/or oral pre- and perioperative steroids is now
commonplace (21).
When using soft surgery, some level of hearing preserva-
tion has been reported in conventional CI recipients with
measureable hearing for the majority of currently available
electrode types, demonstrating that loss of residual hearing
is not an inevitable consequence of cochlear implanta-
tion. For example, Fraysse et al. (22) reported a median low
frequency threshold deterioration of 23dB after one month
in 12 recipients of the Nucleus CI24 device with Contour
Advance electrode, when using a soft surgery protocol.
Obholzer & Gibson (23) reported preservation of residual
hearing in 58 of 81 patients implanted with the Nucleus
CI24 device (straight banded and Contour electrode arrays)
after 6 months follow-up. The mean deterioration of 500Hz
thresholds was 15dB in those with preserved hearing.
Hearing preservation reported for specific electrode types
When hearing preservation is a specific aim, as in candi-
dates for EAS, then most clinical studies have used electrode
arrays designed specifically for hearing preservation. These
arrays are relatively thin, flexible straight arrays designed to
lie along the outer margin of the ST. A substantial number
of studies have quantified the degree of hearing preserva-
tion achieved with specific electrode types, but comparison
among studies is difficult due to a wide range of reporting
methods. Some studies have reported the proportion of
subjects with postoperative low frequency thresholds within
figure 3. Range of post-operative acoustic
thresholds (upper shaded area) suitable for
use of the CP900 processors in EAS mode
Several clinical studies have addressed the indications
for hybrid stimulation in terms of pre-implant hearing
levels. Initially, only subjects with low frequency thresh-
olds poorer than around 65dB HL were implanted (17), but
encouraging early outcomes resulted in relaxation of such
limits. Recent studies have suggested that acoustic ampli-
fication can be effectively provided for low frequency
hearing thresholds down to about 70dB HL at 250Hz. When
thresholds are poorer than this, subjects tend to prefer CI
(electrical) alone stimulation (18). At higher frequencies,
thresholds should be below about 80dB HL (i.e. in line
with indications for conventional CI), as acoustic hearing
aids cannot provide useful listening benefit for such high
frequency hearing losses. However, although these general
audiometric threshold guidelines are relatively clear, there
is considerable heterogeneity in recipient types. Some
individuals have very good low frequency hearing so that
they do not require amplification of low frequencies (19).
Many have substantial hearing levels in the non-implanted
ear and are able to benefit from binaural low frequency
hearing in addition to the mid-high frequency information
provided by the CI.
[Electro-Acoustic Stimulation - an option when hearing aids are not enough - Herbert Mauch Biomed Eng. et al.]