706
Catheter tip position
Poor tip position increases risks of: thrombosis, arrhyth-
mias, perforation of vein wall (causing hydrothorax, cardiac
tamponade, extravasation), catheter failure, pain on injec-
tions, and stenosis. A adequate length of catheter, in long
axis of the SVC, with its tip above the pericardial reflection
is traditionally considered ideal, and this approximates to
the level of the carina. This is often not possible, particu-
larly with left-sided catheters (18). A frequent problem is a
short catheter with its tip abutting vein wall with an acute
angle (Figure 5).
Most practitioners now aim to have catheter tips at the
cavo-atrial junction (two vertebral body units below
carina) (19).
Imaging
Short-term CVCs are usually inserted without real-time
imaging, with a CXR to confirm positioning. Catheter tips
move with changes from lying to sitting/standing, or on
deep breathing (20). ECG guidance or electromagnetic
sensors are increasingly used, but do not confirm either
arterial, venous, and mediastinal placement, or a coiled
tip.
Misplaced catheters
Catheters may be misplaced within the venous system
following an abnormal path to the neck, the arm or across
the midline and need repositioning unless for very short
term use. Alternatively patients may have a normal variant
of anatomy or acquired stenosis of the great veins leading
to misplaced catheters. Catheters are typically easily
recognized in such positions and specialist advice is not
generally required before revision, use or removal.
Catheters may be in an obviously incorrect position outside
the vein or appear to follow an approximate normal path on
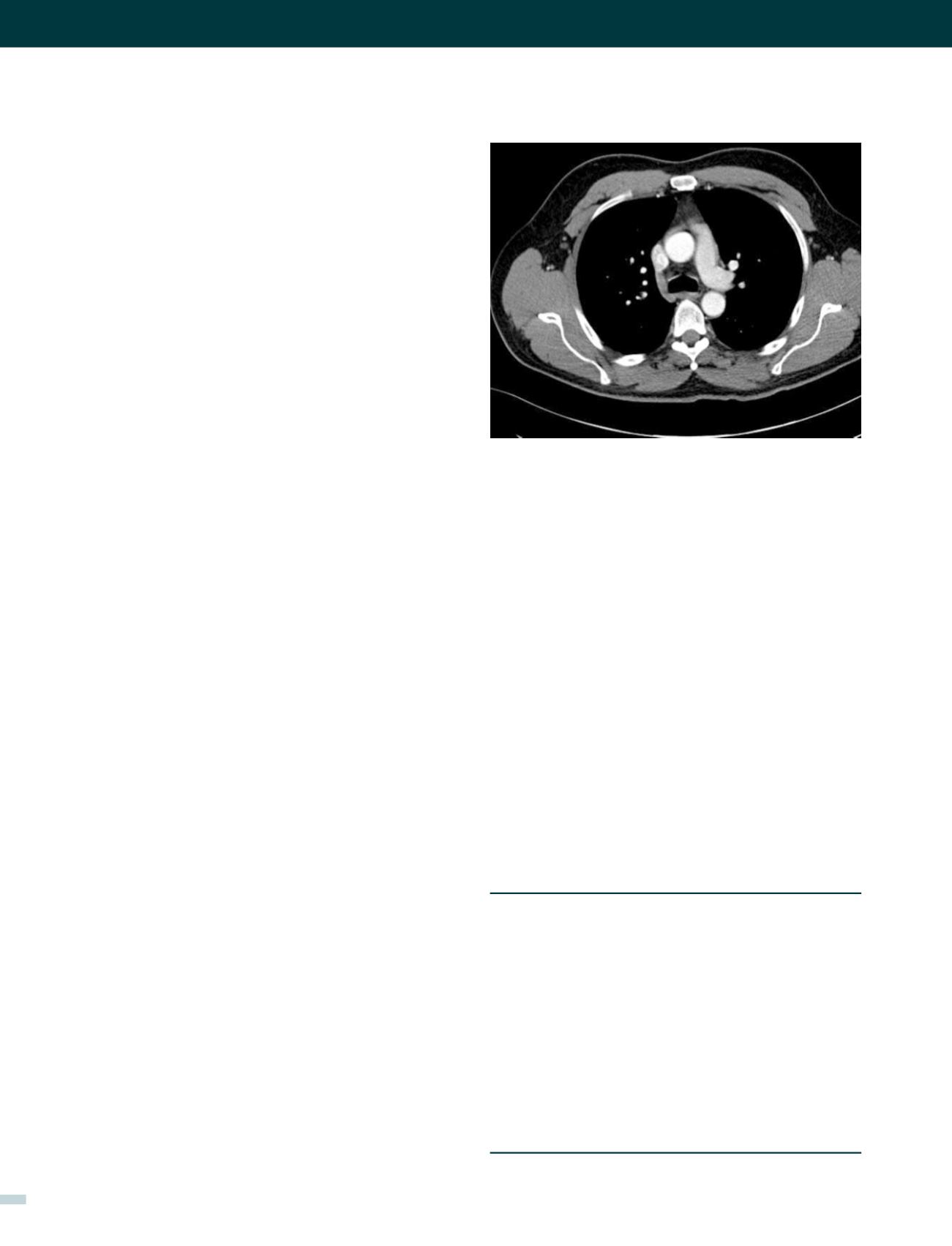
CXR, but are not correctly sited in the SVC. Axial CT images
show how catheters in the SVC, right pleural space, right
internal mammary vessels, azygous system, ascending
aorta, or mediastinum cannot be distinguished on one
plane imaging (Figure 8). CXR can only confirm central
catheter passage, kinking or procedural complications.
Catheters in an unusual position or malfunctioning need
further investigation before use or removal due to the
risks of thrombosis (CVA) if intra-arterial, pneumothorax,
haemothorax or cardiac tamponade. Bedside tests include;
pressures in all lumens (fluid column or transducer), and
aspiration of blood from the lumens for estimation of
haemoglobin (e.g. systemic blood vs pleural collection),
and oxygen partial pressure. None of these bedside tests
•
Early Arrhythmias Vascular injury Pneumothorax
Haemothorax Cardiac tamponade Neural injury
•
Embolization (including guidewire, catheter, or air).
•
Late Infection Thrombosis Embolization
•
Erosion/perforation of vessels
•
Cardiac tamponade
•
Lymphatic damage
•
Arteriovenous fistula.
TABLE 3. COMPLICATIONS OF CVC INSERTION
are entirely reliable. If in doubt, definitive localisation
requires contrast studies (linogram) or cross-sectional CT
imaging (21). “If in doubt, don’t pull it out! seek specialist
advice.
Complications
Any anatomical structure adjacent or connected to vessels
may be damaged during insertion procedures, or later from
thrombosis, perforation, or infection (Table 3) (22).
Some procedural complications are particularly life-threat-
ening and a frequent cause for high- value legal claims
(23,24). These typically relate to local pressure effects from
an arterial haematoma, massive bleeding into the chest/
abdomen, and strokes from carotid cannulation.
FIGURE 8. AXIAL CT O CHEST
This shows how the internal mammary vessels, medial pleura on right,
SVC. ascending aorta, and azygous vein are all similar in anterior to
posterior plane. Catheters in these different structures cannot be dintin-
guished on one plane imaging (CXR).
[REV. MED. CLIN. CONDES - 2017; 28(5) 701-712]
















