703
Landmark techniques
Many techniques of accessing the IJV are described (9).
Typical approaches are from the apex of a triangle enclosed
within the two heads of the sternomastoid. The neck is
gently extended and turned a little to the opposite side.
The carotid artery is felt at the level of the cricoid carti-
lage. The jugular venous pulse may be seen, and the vein if
compressed will on release be seen to refill. The needle is
inserted from the apex of the triangle at an angle of o and
aimed towards the ipsilateral nipple. The vein often collapses
under the needle, which then transfixes it, and puncture
is not recognized. The vessel may then be located by aspi-
rating as the needle is slowly withdrawn. The vein is usually
less than 2cm from skin and can be located with a standard
green ‘seeker’ needle. The vein can be cannulated in the
semi-upright position in the case of heart failure or morbid
obesity, if the venous pressure is high.
Ultrasound guidance
There is strong evidence for use of ultrasound for IJV
access to reduce complications and failures (10). Look for
branches (e.g. facial vein), valves, and the carotid, subcla-
vian, and branches thyrocervical trunk. The thyroid gland
(cysts common) and large lymph nodes are visible. Choose
a puncture site and needle direction to minimize overlap of
vein and arteries.
EXTERNAL JUGULAR VEIN
This site is used acutely when a standard peripheral cannula
is placed under direct vision. CVCs passed via the external
jugular vein traverse angles in fascial layers, which may give
problems passing into the subclavian vein.
SUBCLAVIAN VEIN
Landmark approaches are linked with more risks compared
with the IJV, e.g. pneumothorax and incorrect tip place-
ment. It is more comfortable for the patient and a potentially
cleaner site.
Avoid access on the side of arteriovenous fistulae as there is
high pressure in vein and potential risk to fistula from throm-
bosis.
Landmark techniques
The needle is passed under the clavicle at the junction of
its medial third and lateral two-thirds, and then redirected
towards the suprasternal notch, with continuous aspiration
until blood is seen. The vein may be transfixed, so aspiration
is important on needle withdrawal (11).
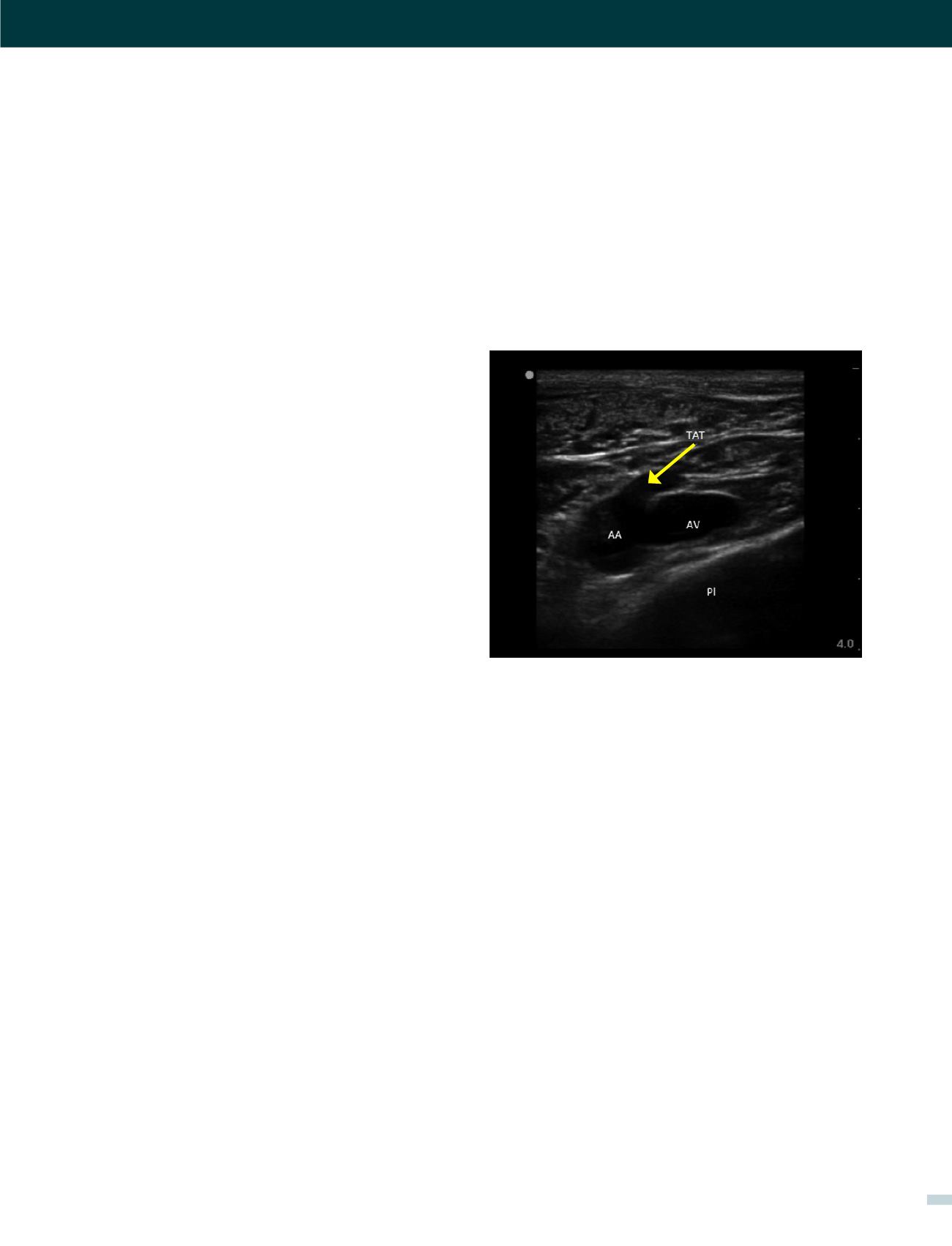
Ultrasound guidance
The clavicle impedes ultrasound, requiring a more lateral
infraclavicular axillary or supraclavicular approach (12).
Recent studies have shown benefits of ultrasound (13,14).
Ultrasound allows avoidance of the nearby pleura, axillary
artery (and the thoracoacromial trunk branches passing
anterior to vein), cephalic vein and brachial plexus (Figure
2). It may be difficult to visualize and access a deep vein in
obese or muscular patients.
FEMORAL VEIN
The anatomy is more complex than the side-to-side orien-
tation of vein and artery in textbooks, which is only relatively
true at the level of the inguinal ligament. Femoral vein access
is useful in patients unable to tolerate head-down position,
in children and emergency situations.
Landmark technique
Palpate the femoral artery and introduce the needle just
medial to the femoral artery close to the inguinal ligament
(not palpable, but represented by a line from iliac crest to
pubis tubercle). It is a common mistake to go too low where
the superficial femoral artery partially overlies the vein.
Ultrasound guidance
Identify the femoral vein and long saphenous vein, and the
common femoral artery dividing into deep and superficial
branches. Higher punctures risk incompressible damage to
vessels, to cause occult bleeding into the peritoneal or retro-
peritoneal space.
[VASCULAR ACCESS - DR. ANDREW BODENHAM]
FIGURE 2. AN ULTRASOUND IMAGE OF RIGHT AXILLARY
VEIN IN MUSCULAR MALE
Note Axillary vein (AV), axillary artery (AA), large thoracoacromial trunk off
axillary artery (TAT), chest wall and pleura (Pl).
















