J.A. Capdevila et al. / Cir Cardiov. 2016;
23(4)
:192–198
193
Prevención de la infección de catéter
Diagnóstico de la infección de catéter
Tratamiento de la infección de catèter
frecuentemente por
Staphylococcus aureus
, lo que explica su gravedad. En este documento de consenso,
elaborado por un panel de expertos de la Sociedad Espa˜nola de Infecciones Cardiovasculares con la cola-
boración de expertos de la Sociedad Espa˜nola de Medicina Interna, la Sociedad Espa˜nola de Quimioter-
apia y la Sociedad Espa˜nola de Cirugía Torácica-Cardiovascular, pretende establecer unes normas para
un mejor uso de los catéteres venosos periféricos de corta duración. El Documento revisa las indica-
ciones para su inserción, mantenimiento, registro, diagnóstico y tratamiento de las infecciones derivadas
y las indicaciones para su retirada; haciendo énfasis en la formación continuada del personal sanitario
para lograr una mayor calidad asistencial. Seguir las recomendaciones del consenso permitirá utilizar de
una manera más homogénea los catéteres venosos periféricos minimizando el riesgo de infección y sus
complicaciones.
© 2016 Publicado por Elsevier Espa˜na, S.L.U. en nombre de Sociedad Espa˜nola de Cirug´ıa
Tor´acica-Cardiovascular. Este es un art´ıculo Open Access bajo la licencia CC BY-NC-ND (http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Background
The use of endovascular catheters is generalized practice in the
hospital setting.
1
A recent prevalence study showed that 81.9%
of patients admitted to Internal Medicine services are inserted
with one or more catheters, out of which 95.4% are short dura-
tion peripheral lines.
2
It has also recently been documented the
increasing influence of peripheral catheters as a driver for nosoco-
mial bacteremia with high associated morbidity and mortality.
3–5
Several studies have shown that the risk of bacteremia related
to a peripheral venous catheter (PVC) is similar to that of cen-
tral venous lines
6
with an estimate of 0–5 bacteremia episodes
per 1000 catheter-days in admitted adult patients.
4,6
Further-
more, the vast majority of cases of PVC-related bacteremia are
S.
aureus
bacteremia; this is different from central venous lines, being
S. epidermidis
the most frequent isolated pathogen in the latter
setting.
3,4
This yields a higher complication rate including nosoco-
mial endocarditis thusmaking treatment difficult. There are several
guidelines and consensus documents on prevention, diagnosis and
treatment of central venous catheter-related infections
7–10
that
have greatly contributed to reduce the infection rate and facilitate
its management, especially in Intensive Care Units (ICU). However,
there is scanty literature focusing on short duration peripheral
catheters which are those mostly used out of the ICU setting.
1,11
Several observational studies have shown that there is lack of
knowledge on how to use PVC by the attending staff
12
and on the
opportunities to improve its handling.
1,12–14
Objective
The objective of this Consensus Document is to review evidence
andmake recommendations formanagement of short duration PVC
in adults. This will allow uniformity in usage thus minimizing the
risk of infection and its complications.
Participating organizations
This Consensus Document has been elaborated by a panel
of experts of the Spanish Society of Cardiovascular Infections
(SEICAV) in cooperation with experts from the following scien-
tific societies: Spanish Society of Internal Medicine (SEMI), Spanish
Society of Chemotherapy (SEQ) and Spanish Society of Thoracic-
Cardiovascular Surgery (SECTCV).
Methods
The recommendations for insertion, handling and removal of
PVCs and also what to do when suspecting infection (diagnosis)
and its treatment are issued based on the best scientific avail-
able evidence or, when not available, on expert opinion. Therefore,
PubMed
(www.PubMed.org)literature search between 1986 and
2015 has been performed. This is awell-known free access resource
established and maintained by the National Center for Biotechnol-
ogy Information (NCBI) of the National Library of Medicine (NLM)
of the USA, which provides free access to MEDLINE, the database
of citations and abstracts of the NLM. It currently stores over
24 million citations from over 5600 biomedical journals.
In our PubMed search using the Medical Subject Head-
ings (MeSH) terms “management of peripheral venous catheter”
(
N
= 363) and “peripheral catheter-related bacteremia” (
N
= 260),
studies related to newborns or pediatric patients and studies
on peripherally inserted central catheters (PICC) were discarded.
MeSH terms is the NLM controlled vocabulary thesaurus used for
indexing articles for PubMed
(www.pubmed.org). Guidelines on
prevention, diagnosis and treatment of catheter infection were
reviewed.
7–10
The levels of evidence and strength of recommendations accord-
ing to the below definitions will be shown in bold within brackets
when a recommendation is made in the text.
Definitions
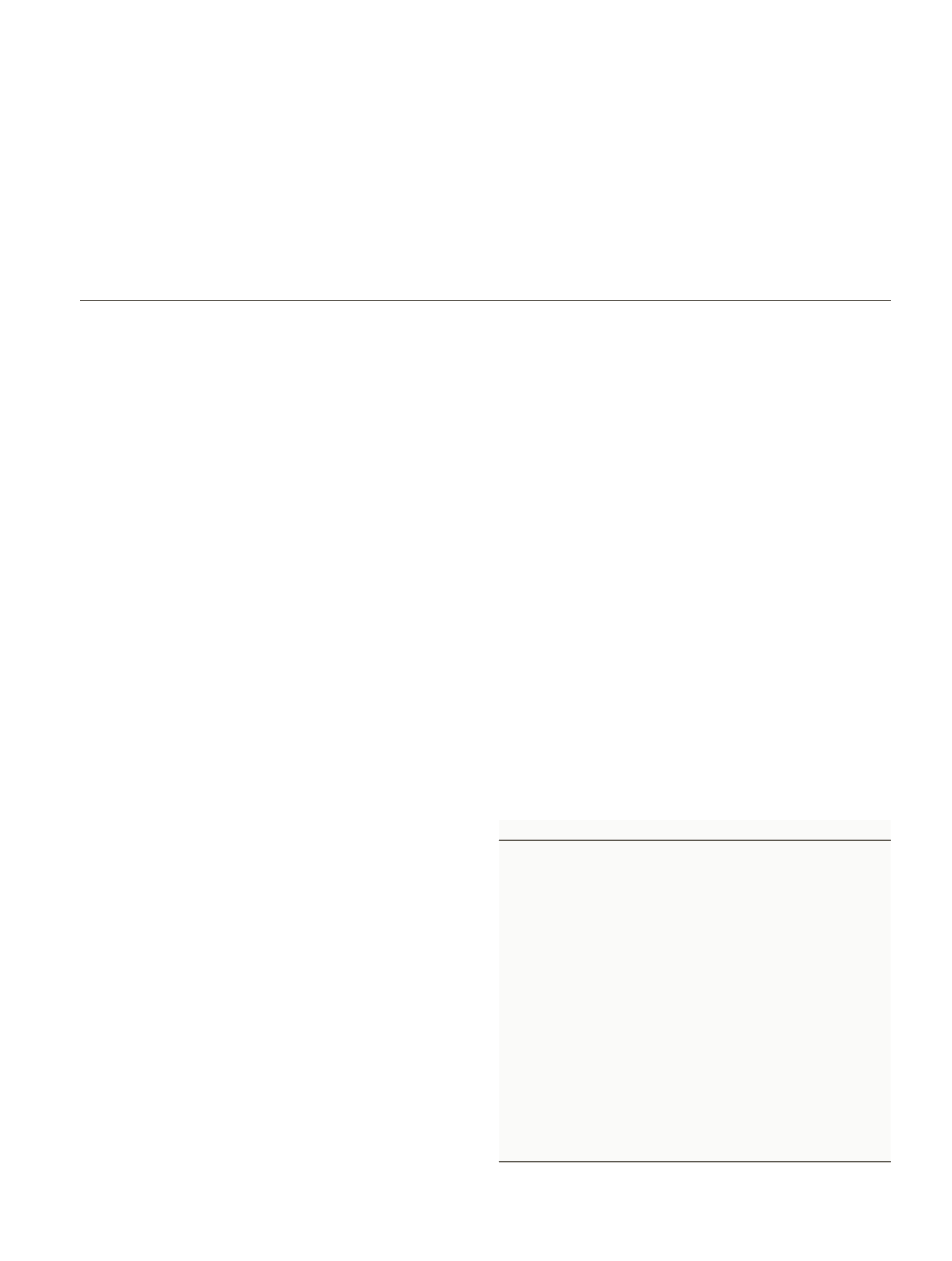
Table 1 describes the levels of evidence and the strength of rec-
ommendations according to the criteria of the Infectious Disease
Society of America (ISDA).
15
PVC is a catheter shorter than 7.62 cm (3 in.).
Table 1
Infectious Disease Society of America – United States Public Health Service Grading
System for ranking recommendations in clinical guidelines.
15
Category, grade
Definition
Strength of recommendation
A
Good evidence to support a recommendation
for use
B
Moderate evidence to support a
recommendation for use
C
Poor evidence to support a recommendation
D
Moderate evidence to support a
recommendation against use
E
Good evidence to support a recommendation
against use
Quality of evidence
I
Evidence from >1 properly randomized,
controlled trial
II
Evidence from >1 well-designed clinical trial,
without randomization; from cohort or
case-controlled analytic studies (preferably
from >1 center); from multiple time-series; or
from dramatic results from uncontrolled
experiments
III
Evidence from opinions of respected
authorities, based on clinical experience,
descriptive studies, or reports of expert
committees