196
J.A. Capdevila et al. / Cir Cardiov. 2016;
23(4)
:192–198
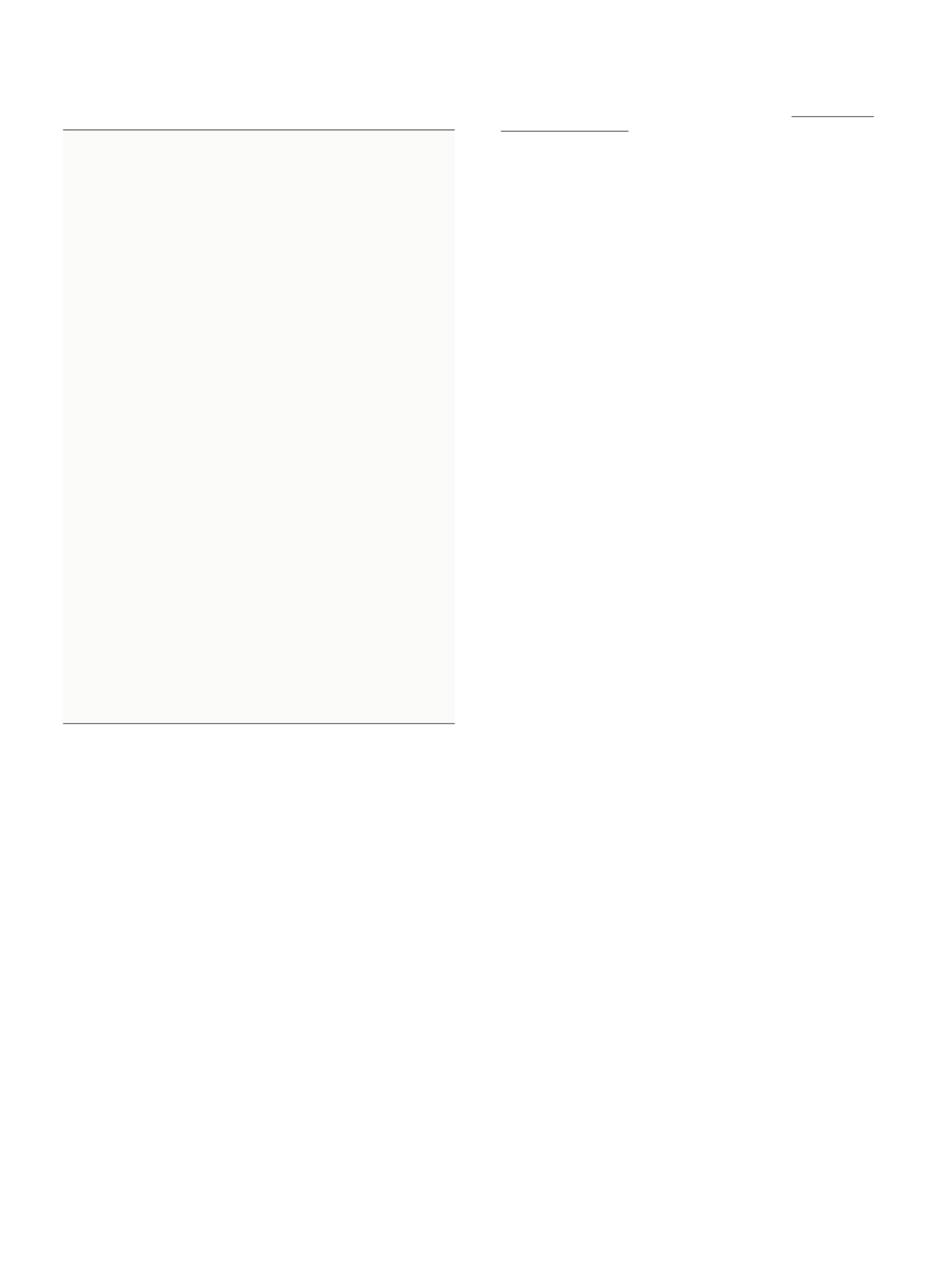
Table 3
Summary of recommendations and degree of evidence and (references) (see - 1).
Always assess the need of inserting a catheter. If necessary,
a central venous line should be preferred over a PVC if
duration of intravenous treatment longer than 6 days or
blood transfusion, parenteral nutrition or chemotherapy.
I-A
17,18
If possible, PVC should not be placed in the lower
extremities or at the elbow crease due to higher risk of
phlebitis.
II-A
20,21
Insertion of PVC must be performed with the maximum
hygiene with no need for a surgical field. There are no
preferences as to which disinfectant solution to use.
I-A
9,22,23
An sterile dressing must be used to cover the insertion site
(gauze dressing or transparent semi permeate).
II-A
24,25
Adherence to pre-insertion checklist improves prevention
of complication outcomes.
I-A
10,31
The need for PVC should be assessed on daily basis. If it is
not necessary, it is advisable to remove the PVC.
II-A
18,32,33
The insertion site must be inspected daily. If abnormalities,
malfunction or discomfort at the subcutaneous site, PVC
should be removed.
III-A
17,34,35
No antiseptic cream/gel should be used at the insertion
site.
III-C
36
Closed connectors to access the PVC can be used; its
external surface must always be decontaminated.
II-A
37
Infusion sets can be utilized up to 96 h, exception made of
blood transfusion or lipid emulsions.
I-A
38,39
It is mandatory that the nursing files a daily record of the
PVC.
III-A
40
It is not advisable to remove PVC on a routine basis. PVC
should be replaced when clinically indicated.
I-A
18,41–51
It is advisable not to keep a PVC in place for over 5 days.
III-B
Unused catheters must be removed.
II-A
10,53,55
When there is suspicion of PVC inserted under suboptimal
conditions, it must be removed.
III-A
56,57
If there is suspicion of infection, it is not indicated to use
diagnostic technique leaving the PVC in place.
III-A
If there is a suspicion of catheter-related infection, the tip
of the PVC must be submitted for Microbiology.
Removed PVC non-suspected to be infected not need
Microbiology.
III-A
Empiric antibiotic treatment of PVC-related bacteremia
has to be deescalated according to microbiology results.
I-A
67,68
Continuous education in insertion and maintenance
guidelines is an appropriate way to reduce
complications.
I-A
74–87
a continuous education program leads to relaxation of the norm,
abandonment of good clinical practices and increase in infection
and complication rates. On the contrary, specific educational pro-
grams help in reducing infection rates.
82–87
There are different
ways to provide education. Education among peers has shown the
best benefits in guideline follow-up as the staff is engaged in edu-
cation.
It is advisable that the infection and complication rates are peri-
odically disclosed to the staff in charge of inserting PVCs. This
is positive reinforcement on guideline/protocol follow-up and a
warning if deviations occur. Furthermore, the adherence to the
checklist can be monitored (Table 2).
Source of funding
No external funding sources.
Conflict of interest
No conflicts of interest declared.
References
1. Pérez-Granda MJ, Guembe MR, Rincón C, Mu˜noz P, Bouza E. A prevalence survey
of intravascular catheter use in a general hospital. J Vasc Access. 2014;25:524–8.
2. Guembe M, Pérez-Granda MJ, Capdevila JA, Barberan J, Pinilla B, Martín-
Rabadán P, et al. Nationwide study of the use of intravascular catheters
in internal medicine departments. J Hosp Infect. 2015,
http://dx.doi.org/10.1016/j.jhin.2015.01.024
3. Pujol M, Hornero A, Saballs M, Argerich MJ, Verdaguer R, Cisnal M, et al. Clinical
epidemiology and outcomes of peripheral venous catheter-related bloodstream
infections at a university-affiliated hospital. J Hosp Infect. 2007;67:22–9.
4. DelgadoM, Gabillo A, Elias L, Yebenes JC, Sauca G, Capdevila JA. Caracteristicas de
la bacteriemia relacionada con catéter venoso periférico en un hospital general.
Rev Esp Quimio. 2012;25:129–33.
5. AlmiranteB,LimónE,FreixasN,GudiolF.Vigilanciadebacteriemiasrelacionadas
con el uso de catéteres venosos en los hospitales de Catalunya. Resultados
del Programa VINCAT (2007–2010). Enf Infecc Microbiol Clin. 2012;30 Suppl.
3:13–9.
6. ChopraV,AnandS,KreinSL,ChenowethC,SaintS.Bloodstreaminfection,venous
thrombosis, and peripherally inserted central catheters: reappraising the evi-
dence. Am J Med. 2012;125:733–41.
7. León C, Ariza X. Guías para el tratamiento de las infecciones relacionadas con
catéteres intravasculares de corta permanencia en adultos: conferencia de con-
senso SEIMC-SEMICYUC. Enf Infecc Microbiol Clin. 2004;22:99–101.
8. Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, et al. Clinical
practice guidelines for the diagnosis andmanagement of intravascular catheter-
related infection: 2009. Update by the Infectious Diseases Society of America.
Clin Infect Dis. 2009;49:1–45.
9. O ´Grady N, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guide-
line for the prevention of intravascular catheter-related infections. Clin Infect
Dis. 2011;52:162–93.
10. Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An
intervention to decrease catheter-related bloodstream infections in the ICU. N
Engl J Med. 2006;355:2725–32.
11. Capdevila JA. El catéter periférico: el gran olvidado de la infección nosocomial.
Rev Esp Quimioter. 2013;26:1–5.
12. Cicolini G, Simonetti V, Comparcini D, Labeau S, Blot S, Pelusi G, et al.
Nurse’s knowledge of evidence-based guidelines on the prevention of periph-
eral venous catheter-related infections: a multicentre survey. J Clin Nurs.
2014;17–18:2578–88.
13. Ahlqvist M, Beerglund B, Wiren M, Klang B, Johansson E. Accuracy in documen-
tation – a study of peripheral venous catheters. J Clin Nurs. 2009;13:1945–52.
14. Véliz E, Vergara T, Fica A. Evaluación de las condiciones de manejo de
catéteres vasculares periféricos en pacientes adultos. Rev Chilena Infectol.
2014;31:666–9.
15. Kish MA. Guide to development of practice guidelines. Clin Infect Dis.
2001;32:851–4.
16. American College of Chest Physicians/Society of Critical Care Medicine. Consen-
sus Conference: definitions for sepsis and organ failure and guidelines for the
use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
17. Maki D, Ringer M. Risk factors for infusion-related phlebitis with small
peripheral venous catheters. A randomized controlled trial. Ann Intern Med.
1991;114:845–54.
18. Mestre G, Berbel C, Tortajada P, Gallemí G, Aguilar M, Caylà J, et al. Assessing the
influence of risk factors on rates and dynamics of peripheral vein phlebitis: an
observational cohort study. Med Clin. 2011;139:185–91.
19. Göransson KE, Johansson E. Indication and usage of peripheral venous catheters
inserted in adult patients during emergency care. J Vasc Access. 2011;3:
193–99.
20. Dunda S, Demir E, Mefful O, Grieb G, Bozkurt A, Pallua N. Management, clinical
outcomes, and complications of acute cannula-related peripheral vein phlebitis
of the upper extremity: a retrospective study. Phlebology. 2014;30:381–8.
21. Uslusoy E, Mete S. Predisposing factors to phlebitis in patients with periph-
eral intravenous catheters: a descriptive study. J Am Acad Nurse Pract.
2008;20:172–80.
22. Maki DG, Ringer M, Alvarado CJ. Prospective randomized trial of povidone-
iodine, alcohol, and chlorhexidine for prevention of infection associated with
central venous and arterial catheters. Lancet. 1991;338:339–43.
23. Canadian Agency for drugs and technology in health. Use of chlorhexidine
gluconatewithalcoholforthepreventionofperipheralintravenousdeviceinfec-
tions: a review of clinical and cost effectiveness and guidelines; 2014, April
3.
24. Maki DG, Stolz SS, Wheeler S, Mermel LA. A prospective, randomized
trial of gauze and two polyurethane dressings for site care of pulmonary
artery catheters: implications for catheter management. Crit Care Med.
1994;22:1729–37.
25. Bijma R, Girbes AR, Kleijer DJ, Zwaveling JH. Preventing central venous catheter-
related infection in a surgical intensive-care unit. Infect Control Hosp Epidemiol.
1999;20:618–20.
26. Göransson KE, Johansson E. Prehospital peripheral venous catheters: a prospec-
tive study of patients complications. J Vasc Access. 2012;13:16–21.
27. Forni C, Loro L, Tremosini M, Trofa C, D’Alessandro F, Sabattini T, et al.
Cohort study of peripheral catheter-related complications and identification
of predictive factors in a population of orthopedic patients. Assist Inferm Ric.
2010;29:166–77.
28. Aulagnier J, Hoc C, Mathieu E, Dreyfus JF, Fischler M, Le Guen M. Efficacy of
accuvein to facilitate peripheral intravenous placement in adults presenting
to an emergency department: a randomized clinical trial. Acad Emerg Med.
2014;21:858–63.
29. Au AK, Rotte MJ, Grzybowski RJ, Ku BS, Fields JM. Decrease in central venous
catheter placement due to use of ultrasound guidance for peripheral intravenous
catheters. Am J Emerg Med. 2012;30:1950–4.