621
conversion into an active form is not required and the active
drug component is immediately available. Subsequently, a
loading dose of polymyxin B should achieve an active peak
concentration immediately. When used in combination
with larger daily doses, the ƒAUC/MIC can more easily be
maximized. Current dosing recommendations for polymyxin
B max out at 1.5 to 2.5mg/kg per day. However, a recent
pharmacokinetic study in 24 patients demonstrated that
a loading dose of 2.5mg/kg as a 2 hour infusion, followed
by 1.5mg/kg every 12 hours as 1 hour infusions, would
achieve a total daily AUC of
~
50mg*h/L in approximately
90% of patients (36). This exposure would be sufficient to
obtain the ƒAUC/MIC target of 12 up to MICs of 2mg/L.
Notably, polymyxin B
clearance
is not significantly affected
by reductions in creatinine
clearance
, so aggressive
dosage adjustments in this population are not required. A
retrospective study by Nelson and colleagues (37) in patients
with bloodstream infections due to carbapenem-resistant
gram-negative rods observed that receipt of polymyxin
B daily doses
<
1.3mg/kg was significantly associated with
30-day mortality (OR=1.58; 95% CI 1.05 to 1.81; P=0.04).
Furthermore, patients with renal impairment made up 82%
of those receiving reduced polymyxin B doses.
While the above data with colistin and polymyxin B are
promising to guide optimal dosing, adaptive resistance
remains a challenge. An
in vitro
pharmacodynamic study
with several
A. baumannii
clinical isolates demonstrated
significant regrowth of the total population, due to
the emergence of adaptive resistance in all strains (38).
This occurred even in the presence of aggressive dosing
regimens (i.e., simulating free steady-state average
concentrations of 3mg/L). Adaptive resistance to the
polymyxins has also been described with
P
.
aeruginosa
and
Enterobactericeae
. As a result, optimal dosing of polymyxins
is encouraged, but unlikely to result in promising clinical
response when administered alone, and combination
therapy is routinely recommended.
THE VALUE OF THE MIC
A common theme from the above review of pharmacodynamic
concepts for all antibiotics is the importance of MIC. When
determining an optimized dosing regimen to implement in
the hospital setting, the ASP should consider local resistance
rate trends. Furthermore, several studies have stressed
the importance of institution specific data. While general
susceptibility patterns can be identified from a hospital
antibiogram, details on the MIC distributions of organisms
are frequently absent.
True antibiotic MIC testing is uncommonly conducted by most
microbiology laboratories because it is more labor intensive
and costly than automated (Vitek II™, Microscan™, etc.)
susceptibility testing alone. Additionally, most prescribers
have not received training to properly interpret the MIC. For
these reasons, the microbiology laboratory typically only
conducts breakpoint testing, which is synonymous with
MIC testing but over only a small range of dilutions around
the susceptibility and resistance breakpoints. For example,
if an antibiotic’s susceptibility and resistance breakpoints
are
≤
8mg/L and
≥
32mg/L, respectively, most automated
systems will only test these concentrations. If the bacteria
do not grow at 8mg/L, then “susceptibility” is reported. It
cannot be determined, however, if the MIC is 8mg/L (i.e.,
borderline susceptible) or much lower (e.g., 0.5mg/L).
Likewise, if the organism grows at both concentrations (8
and 32mg/L), then it is reported as resistant, but clearly
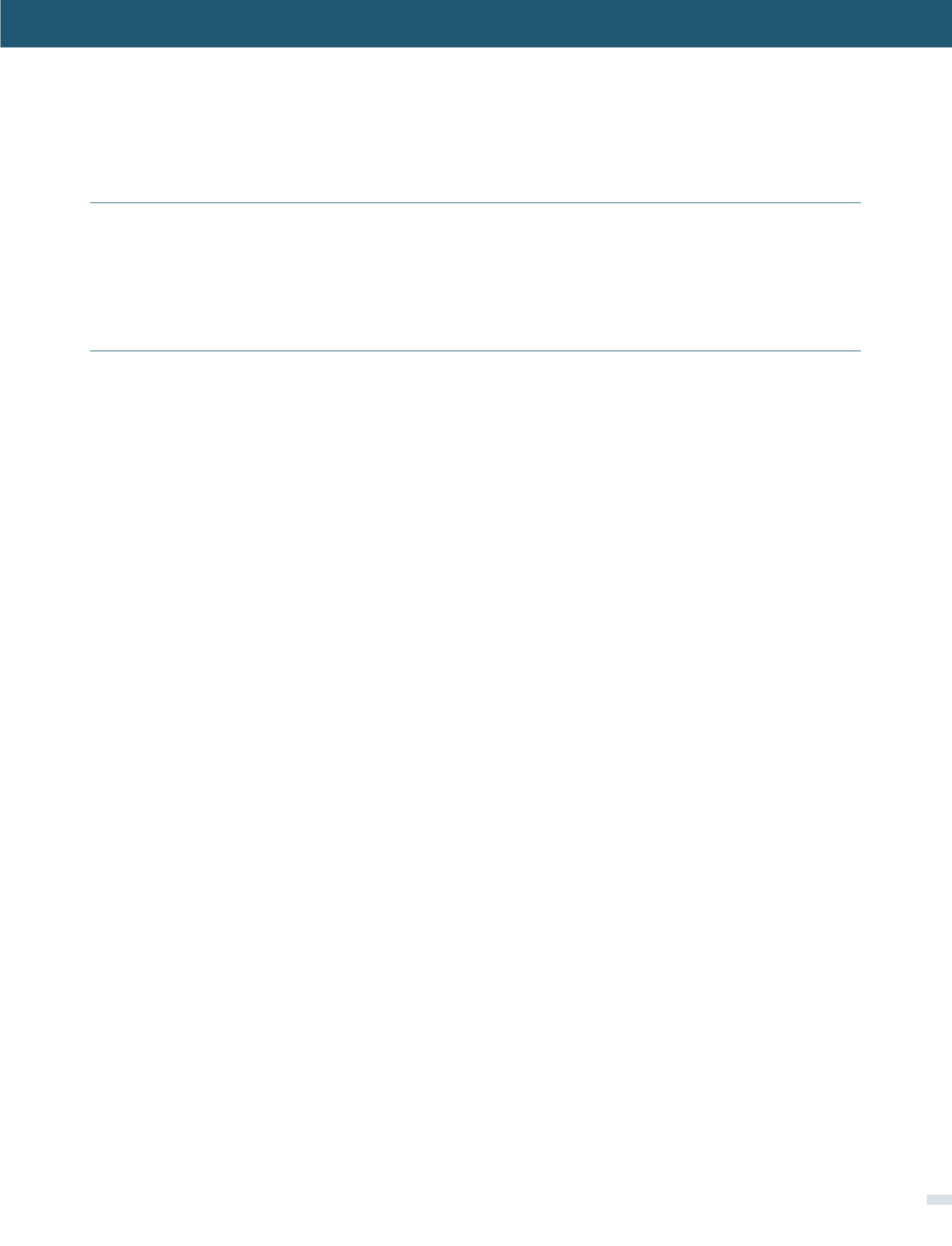
TABLE 2. UPDATED US FOOD AND DRUG ADMINISTRATION (FDA) AND EUROPEAN MEDICINES AGENCY (EMA)
DOSING RECOMMENDATIONS FOR INTRAVENOUS COLISTIMETHATE BY CREATININE
CLEARANCE
RANGE
CBA:
colistin base activity (1mg of CBA = 2.4mg of colistimethate sodium = 30,000 IU; each colistimethate sodium vial contains 150mg CBA); MIU: million
international units
a
FDA expressed doses in mg/kg of CBA, using actual body weight except in obese individuals, where the dosage should be based on ideal body weight.
Doses are divided into 2-3 doses per day. No recommendation for a loading dose is made.
b
EMA expresses doses in MIU, which have been converted to mg of CBA for this table. Doses are divided into 2-3 doses per day. The EMA recommends
a loading dose of 9 MIU (~300mg CBA) in critically ill patients.
c
EMA indicates that daily doses up to 12 MIU (~400mg CBA) may be required for patients with good renal function.
CREATININE
CLEARANCE
(ML/MIN)
US FDA
DAILY DOSE
a
EMA
DAILY DOSE
b
≥
80
2.5-5mg CBA/kg
9 MIU (
~
300mg CBA)c
50 to
<
80
2.5-3.8mg CBA/kg
9 MIU (
~
300mg CBA)c
30 to
<
50
2.5mg CBA/kg
5.5-7.5 MIU (
~
183–250mg CBA)
10 to
<
30
1mg CBA/kg
(or 1.5mg CBA/kg every 36 hours)
4.5-5.5 MIU (
~
150-183mg CBA)
<
10
NA
3.5 MIU (
~
117mg CBA)
[OPTIMIZING ANTIMICROBIAL PHARMACODYNAMICS: A GUIDE FOR YOUR STEWARDSHIP PROGRAM - Joseph L. Kuti, PharmD]